When I started writing my recent article on COVID-19 testing, I assumed that I would be doing a compare and contrast sort of article. Like many people, I assumed that the “gold standard” test would be the reverse transcriptase-polymerase chain reaction (RT-PCR) test that I described in some detail. And indeed it is, but it’s not without its problems, such as the lack of certified labs and the need for trained technicians to run the samples. I also assumed there would be another test, a simple serological test that could use antibodies to discern if there was an active or even a previous, resolved infection.
At the time I wrote the first article, I could find no indication of an immunologic test for COVID-19 (more specifically, a test for SARS-Cov-2, the virus that causes COVID-19). But almost as rapidly as the number of COVID-19 cases rises, the news changes, and it appears that simple, rapidly performed antibody tests are now or soon will be available. They likely won’t replace the gold standard RT-PCR test, but they do stand to be a game-changer for the front line providers and the victims of this disease. So it pays to take a quick look at immunoassays for infectious diseases, and learn how they work.
Innate and Adaptive
To understand how immunoassays work, it’s necessary to know a little bit about how the human immune system recognizes invaders and targets them for destruction. It’s a vastly complex system, of course, seeing as it is tasked with differentiating between self and non-self cells based on only the slimmest of clues, and a full treatment would take far more time than is needed to get the idea. So yes, this is an extremely stripped-down tour of the immune system, but it should suffice for the task.
Since the main job of the immune system is to recognize and destroy invaders ranging from bacteria to viruses and even other human cells, it has to have something to key on that allows it to be both extremely selective and very aggressive. Proteins, with nearly infinite variability thanks to being composed of 21 different amino acids, make a perfect target, and doubly so since the exteriors of most invaders bristle with dozens of different proteins.
An immune response starts with the innate immune system, a rapid-acting set of first responder cells. The innate system is non-specific; beyond the ability to differentiate between self and non-self, its cells will pretty much eat anything. When it does encounter a bacterium or virus particle, it envelops it and breaks it down, a process known as phagocytosis. All those proteins that were studding the surface of the invader are then presented to another set of cells that form a second immune system, the adaptive immune system.
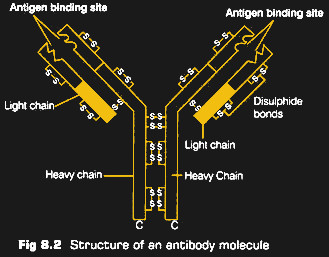
The cells of the adaptive system have their own proteins on the surface, formally referred to as immunoglobulins (Ig) but commonly known as antibodies. These proteins are always shown in diagrams as a Y shape, which is actually pretty accurate. The “arms” of the Y are highly diverse, with different antibodies having different sequences of amino acids. This produces a population of antibodies with varying affinities for other proteins, depending on the size, shape, and electrostatic charge of the amino acids.
When the innate immune cells present the bits and pieces of an invader’s proteins to the adaptive system, with any luck, one of the antibodies will randomly match and bind to the invader. This starts a cascade of events that cause the genes that encoded the matching antibody to be massively amplified in a process called clonal expansion. Cells of the immune system can take days to weeks to mount this defense, but once it starts, a huge number of cells go on patrol, armed with antibodies specific for the infection. Once the invaders are swept up, most of this army of cells is demobilized, but a few memory cells hang on to that specific antibody, ready to mount the offensive rapidly through the innate immune system if the same challenge arises again.
Going With the Flow
Monitoring the state of the immune system, therefore, can tell us not only if a patient is currently fighting an infection, but by digging into the institutional memory of the immune system, it can also tell us if someone has ever faced a specific challenge. All of this requires that we have a sample of the specific antibodies that have been produced by the body as it mounts its defense against a virus. Traditionally, that has been a slow and difficult process, where cells from animals challenged with the virus are painstakingly cultured and amplified through human cell lines, with the resulting antibodies purified before being made available for use in immunoassays.
Antibody purification usually takes months, but in the case of COVID-19, the first antibodies were isolated very quickly. An-Suei Yang et al at the Academia Sinica in Taiwan raised a monoclonal antibody (mAb) against the N, or nucleocapsid, protein of the virus. It took them just 19 days to isolate and purify the antibodies, using a process involving artificial intelligence models of the interactions of antibodies and antigens. Predictions from the model allowed them to create a library of DNA sequences coding for antibodies that should have specificity for the N protein, which can be produced and selected without having to run them through animals first. They managed to cut two months off the usual time to produce an antibody, and have gone on to create others that are so specific for SARS-CoV-2 that they will not bind to any other human coronavirus.
Putting the purified mABs to work in a usable assay is another challenge, and multiple companies are working around the clock to perfect their version of a test. Most of these tests, which are called point-of-care (POC) tests, use the lateral flow architecture. Pregnancy tests are a common example of a lateral flow immunoassay, and are very similar to the COVID-19 POC tests that are soon to hit the market.
Lateral flow tests work by taking a sample from a patient, probably blood for COVID-19 tests, and applying it to an absorbent matrix. The matrix is generally nitrocellulose, through which the blood will rapidly move thanks to capillary action. On its way through the matrix, the sample will cross a region filled with dried buffer reagents and a special mix of antibodies. These antibodies are not necessarily specific for SARS-CoV-2 proteins; they’ll stick to pretty much every protein in the sample. But they are conjugated to some sort of particle, like a colloidal gold microbead or a dyed latex particle. These will provide the visual signal later on in the test.
After crossing the conjugate region of the test, the proteins in the sample are now “decorated” with microparticles. The continue migrating up the strip until the cross lines containing dried mAbs specific for SARS-CoV-2 proteins. Depending on the test format, there could be two or three viral antibodies in these test lines, plus at least one control line that pretty much reacts with anything. Any of the decorated viral proteins in the sample will bind to the test lines, with the accumulation of conjugate producing a colored line that’s easily visible against the background of the matrix.
It’s important to note that there’s also a backdoor technique. Rather than raising up antibodies against SAR-CoV-2 proteins, cloned fragments of viral proteins can be used instead. In this case, the proteins would be applied to the test strips and would bind any conjugated-decorated antibodies in the patient sample. The main advantage here is that mAbs against the viral proteins are not needed, with the disadvantage being that different patients will express higher or lower amounts of antibodies depending on where they are in the viral infection cycle, as well as their general immune response.
Running and interpreting lateral flow immunoassays takes very little training, and the results are generally available within 20 minutes or so. Compared to the hours needed for a qPCR assay, not to mention the certified labs and the time needed to ship samples to them, the benefits of a point-of-care immunoassay are obvious.
Currently, there are at least nine lateral flow immunoassays for various SARS-CoV-2 proteins being developed. Some of them are shipping, some are in validation, and some are seeking approval from regulators. But all of them are based on the amazing complexity and adaptability of the immune system, the system that’s tasked with keeping humans alive in a world where challenges come is the smallest and most insidious packages imaginable.

No comments:
Post a Comment